Chronic Abdominal Pain
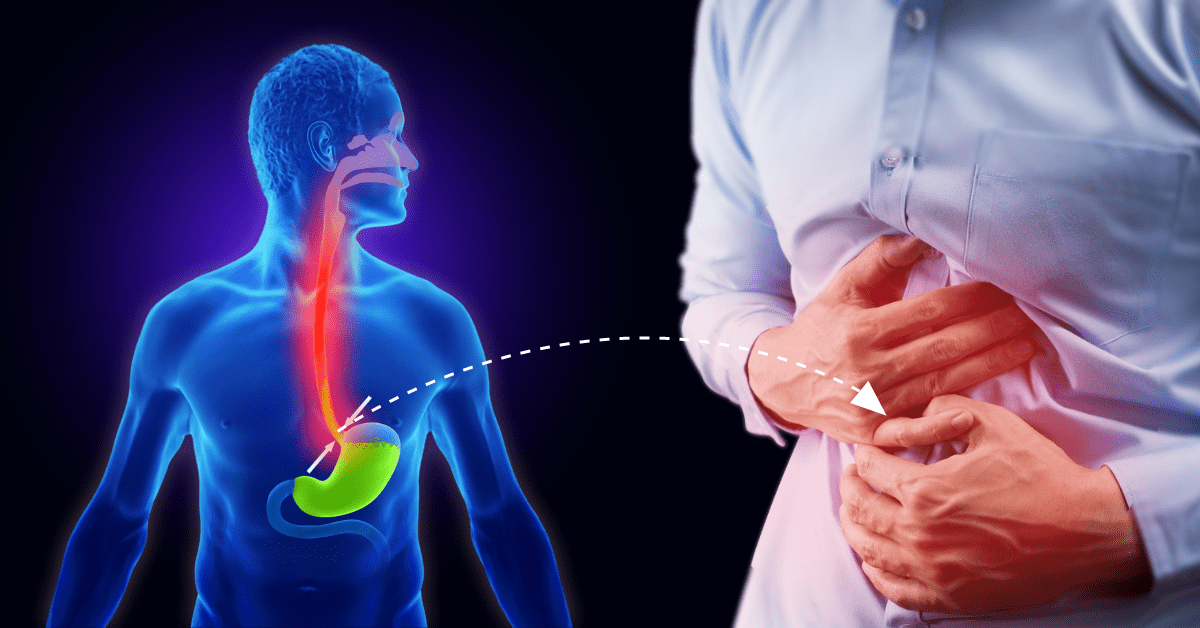
Chronic Abdominal Pain is a type of pain that has existed for more than 6 months and is associated with no specific evidence of a particular disease or condition. This pain is neither associated with bodily functions like bowel movements, eating or menstruation; nor is it associated with medication or toxin. Chronic Abdominal Pain can be categorized into Non-Cancer related abdominal pain, or Cancer-related Abdominal Pain.
Pain receptors in the abdomen respond to mechanical and chemical stimuli. Stretch is the principal mechanical stimulus involved in visceral pain and is brought on by distension and contraction. Different types of chemical and physical causes can work together to make you feel abdominal pain and the threshold for perceiving pain varies among patients. Chronic pain may be triggered by an initial insult, and for some people, normal physiological processes such as digesting food can be felt as painful. Visceral hyperalgesia may predispose to chronic pain even after the initial cause has resolved.
Pain originating in the organ walls can often be perceived to come from a distant site, this is known as referred pain. Referred pain usually is located in the skin’s dermatomes at the causative organ’s spinal levels, or can be from an organ pushing on a nerve that travels elsewhere in the body and causes pain at the distal site. A classic example of this pain is an inflamed gallbladder being perceived as aching scapula (posterior shoulder).
Cancer-related Chronic Abdominal Pain
If your chronic abdominal pain is related to cancer, some treatments that could decrease the intensity of your pain are:
- Intra-thecal pumps for pain medication
- Celiac plexus block
- Splanchnic nerve block
- Spinal Cord Stimulators implant
Non-cancer Related Chronic Abdominal Pain
How can this be treated?
- Intra-thecal pumps for pain medication
- Celiac plexus block
- Splanchnic nerve block
- Spinal Cord Stimulators implant
Conditions
- Arthritis
- Cancer Pain
- Chronic Pelvic Pain
- Chronic Abdominal Pain
- Cervical Radiculopathy
- Complex Regional Pain Syndrome
- Compression Fractures of the Spine
- Diabetic Neuropathy
- Fibromyalgia
- Herniated Discs
- Knee Pain
- Low Back Pain
- Migraine Headaches
- Neck Pain
- Neuropathy
- Post Laminectomy Syndrome
- Shoulder Pain
- Trigeminal Neuralgia
- Whiplash CAD
Treatments
- Botox Injection
- Capsaicin (8%) Patch
- Cervical Epidural Steroid Injection
- Disc Nucleoplasty
- Dorsal Root Ganglion Stimulator (DRG)
- Endoscopic Discectomy
- Facet Joint Syndrome
- Hip Joint Injections
- Intrathecal Pain Pump
- Intercostal Nerve Block
- Ketamine Infusion
- Knee Joint Injection
- Kyphoplasty
- Lidocaine Infusion
- Lumbar Epidural Spinal Injection (LESI)
- Lumbar Sympathetic Ganglion Block
- Lumbar Radiofrequency Neurotomy
- Minuteman Procedure
- Medial Branch Block (MBB)
- Minimally Invasive Lumbar Decompression (MILD)
- Platelet Rich Plasma
- Peripheral Nerve Stimulation
- ReActiv8 Procedure
- Radiofrequency Ablation (RFA)
- Regenerative Medicine
- SI Joint Injection
- Stellate Ganglion Block
- Sympathetic Nerve Block
- Spinal Cord Stimulation (SCS)
- Spinal Stenosis
- Trigger Point Injection
- Transforaminal Epidural Spinal Injection (TFESI)
- Vertebroplasty
- Vertiflex Procedure
